Breathing causes, diagnoses, and treatments
Click a heading to expand it’s content.
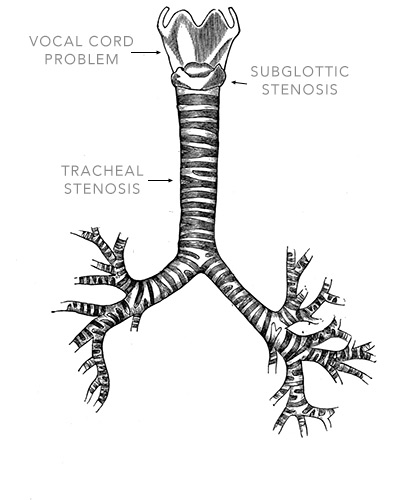
Anatomy
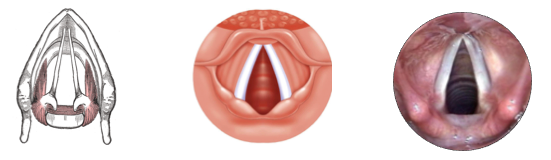
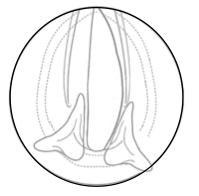
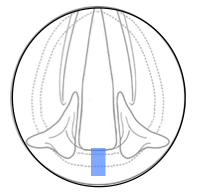
The vocal cords are paired folds of pliable soft tissue attached to cartilage. These cartilages function as articulating joints that move based on paired movements of several delicate muscles. these muscles are primarily controlled by 1 nerve (the recurrent laryngeal nerve).
Open (breathing)
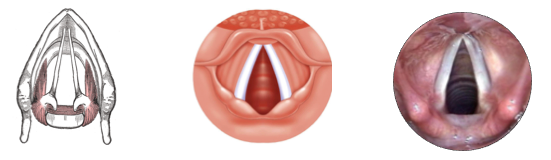
Closed (Talking, Swallowing)
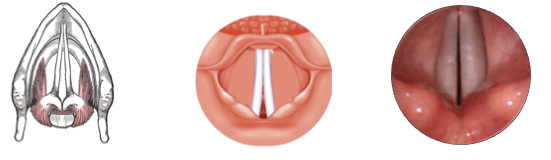
If the vocal cords can’t open, or the opening is blocked, an individual can’t breathe.
Causes
The opening at the top of the trachea (windpipe) can be blocked by diseases of the vocal cord lining:
-
Uncontrolled growths
- · These can be non-cancerous – such as recurrent respiratory papilomatos (RRP)
- · Alternatively, they can arise for cancer – usually squamous cell carcinoma
-
Infiltrative disease
- · Amyloidosis
- · Sarcoidosis
-
Swelling
- · From allergy or infection
-
Broken wiring
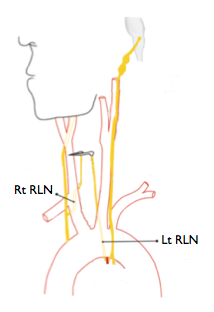
Neurologic injury (specifically injury to the recurrent Laryngeal Nerve: RLN)
The recurrent Laryngeal Nerves run for the base of the brain into the chest before returning up to vocal cord. They can be injured anywhere along their course. Isolated injury to only one nerve will affects voice and swallowing, but injury to both nerves will limit breathing.
Bilateral recurrent laryngeal nerve injuries leave the vocal folds closed and patients suffer with significant shortness of breath and demonstrate stridor. They often end up with a tracheostomy in the acute situation.
This injury can happen from neck trauma (i.e. severe clothesline injuries), but is most often seen as a complication of thyroid surgery. -
Joint Arthritis
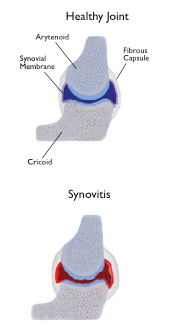
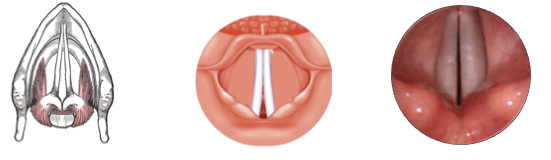
Inflammation and scar in the articulating joints of the vocal cords (the cricoarytenoid joint: CAJ).
CAJ arthritisis a rare cause of vocal cord paralysis. It can result from collagen vascular disease (rheumatoid arthritis, lupus erythematosus), infections(gout, mumps, tuberculosis, syphilis, gonorrhoea) and trauma.
As a result of tissue injury the joint lining becomes inflamed and irregular and no longer glides smoothly. Over time the 2 surfaces can fuse together completely. -
Restrictive Scar
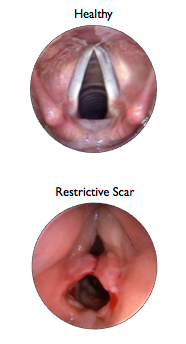
Dense fibrous tissue tethering the 2 vocal cords together
This mostly happens after a breathing tube has been in place for some time (post-intubation).
Early scar tissue from abrasion injury to the delicate airway lining can coalesce to form adhesions between the vocal cords.
Over weeks to months this scar becomes though and thickened limiting vocal cord movement and making it difficult for patients to breathe.
Problems with the small joint responsible for vocal movement can also lead to breathing trouble. The three primary mechanisms of vocal cord immobility related to the joints are:
Treatment
The management of bilateral vocal fold mobility impairment remains an unsatisfactory compromise between voice, breathing and swallowing. As described by a surgeon in 1939, “The desire to get away from the tracheotomy tube has been the father of all operations devised for the relief of bilateral vocal cord paralysis”
Numerous surgical procedures have been proposed to rehabilitate the patient with vocal cord immobility and allow for decanulation. However, the mainstay of surgical therapy over the last 70 years has simply been to enlarge the space between the vocal cords.
This has been accomplished (with minor variations over time), with three basic procedures.
1. Physical lateralization of one (or both) vocal fold(s),
2. Ablative augmentation of the posterior glottis (Cordotomy)
3. Lumen augmentation through posterior cricoid expansion
Due to the rarity of bilateral vocal cord paralysis, the three basic surgical approaches are used without good studies to assess their effectiveness at avoiding tracheostomy, or their associated sided effects. It remains unclear which type of procedure is best suited to each individual. The lack of an ideal solution is aptly illustrated by the abundance of technical reports in the literature over the last 100 years.
Current techniques improve breathing at the expense of voice.
Many investigators have tried restoring lost neural signal in patients with nerve injuries. Although an area of rapid progress and active development, to date clinically, laryngeal re-innervation has rarely restored vocal cord movement.
Another promising line of research for patients with neurologic injuries is implantable stimulators. These may restore maintain mobility and voice patterns, but they have not yet become a mainstream option available to patients outside of experimental studies.

Here's what's happening with NoAAC:
The 2016 AAO-HNSF Annual Meeting & OTO EXPO will be held Sunday, September 18 - Wednesday, September 21, 2016 in San Diego, CA. For additional information on this year's Annual Meeting, please visit: http://www.entannualmeeting.org/16. Check...
During the annual Combined Otolaryngology Spring Meeting in Chicago, Illinois, NoAAC investigators are invited to attend a meeting and reception at The Gage restaurant on Thursday, May 19 from 11am-2pm. The Gage restaurant is located at 24 S Michigan Ave, about 5 blocks south of the COSM conference...
The Inaugural North American Airway Collaborative Symposium on Advanced Surgical Techniques in Adult Airway Reconstruction was held on February 22, 2016 in Baltimore, Maryland.
Click here to view the Program Announcement
The NoAAC Network is holding a trial meeting concurrent with the American Academy of Otolaryngology-Head & Neck Surgery annual meeting in Dallas, Texas September 28th from 1-2pm in the Aloft Hotel....
